Talk to your doctor if you or someone close to you has symptoms of Frontotemporal dementia.
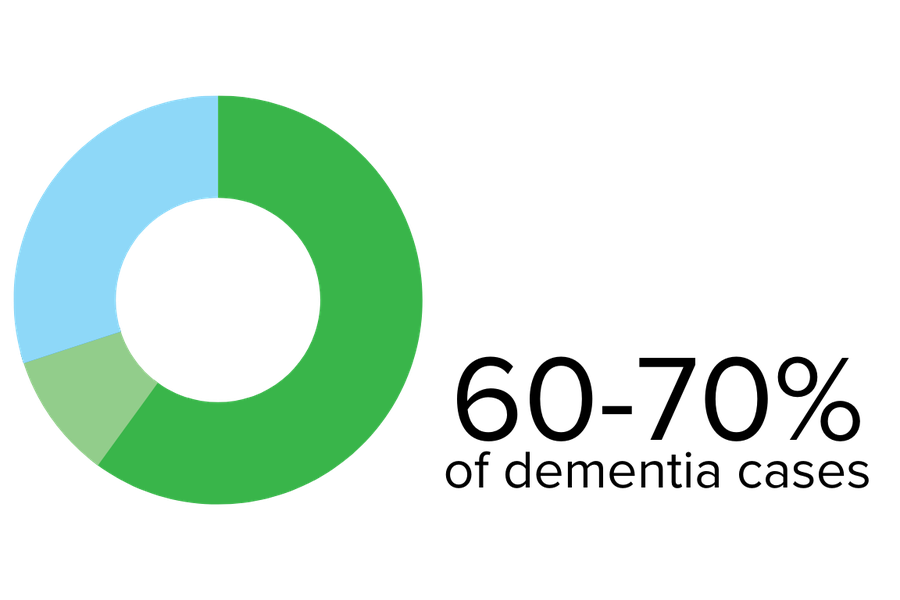
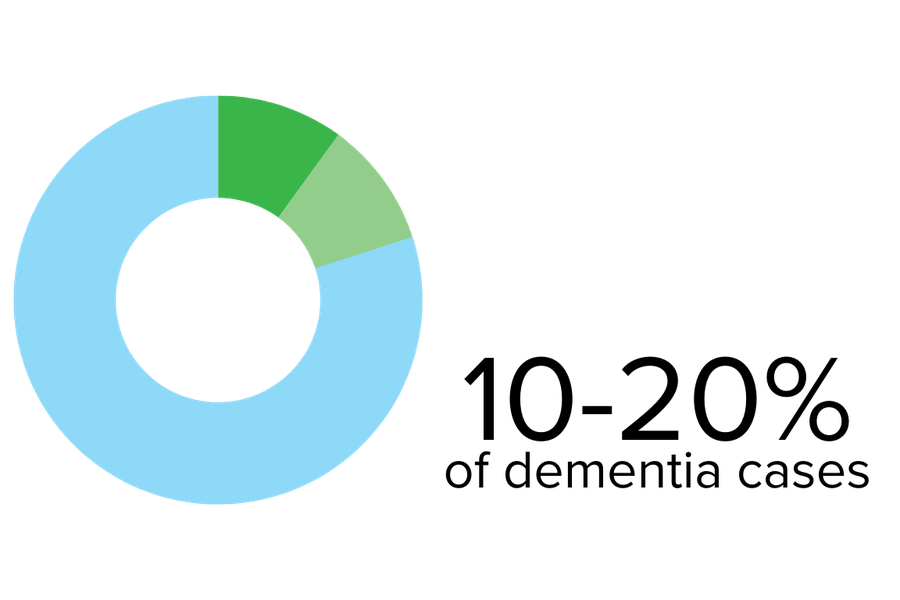
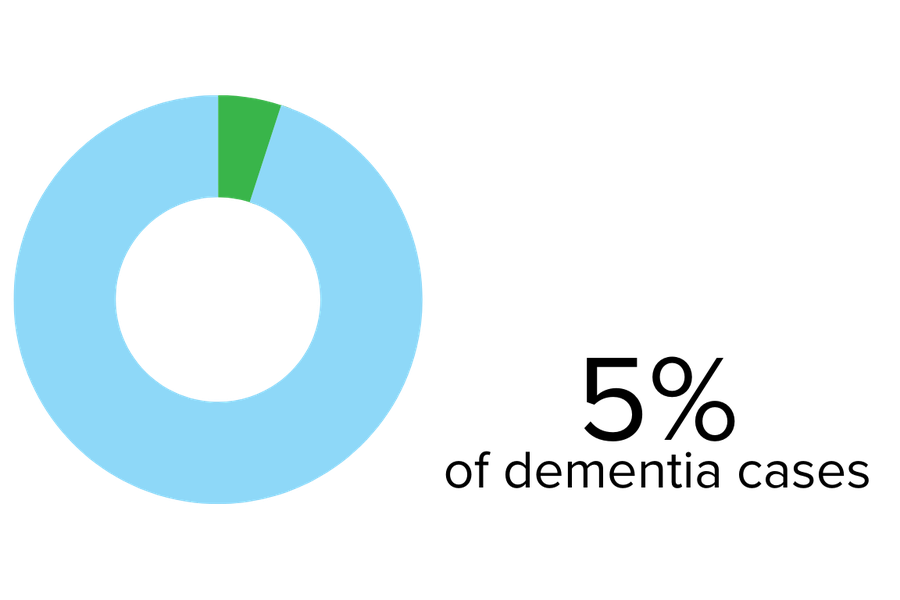
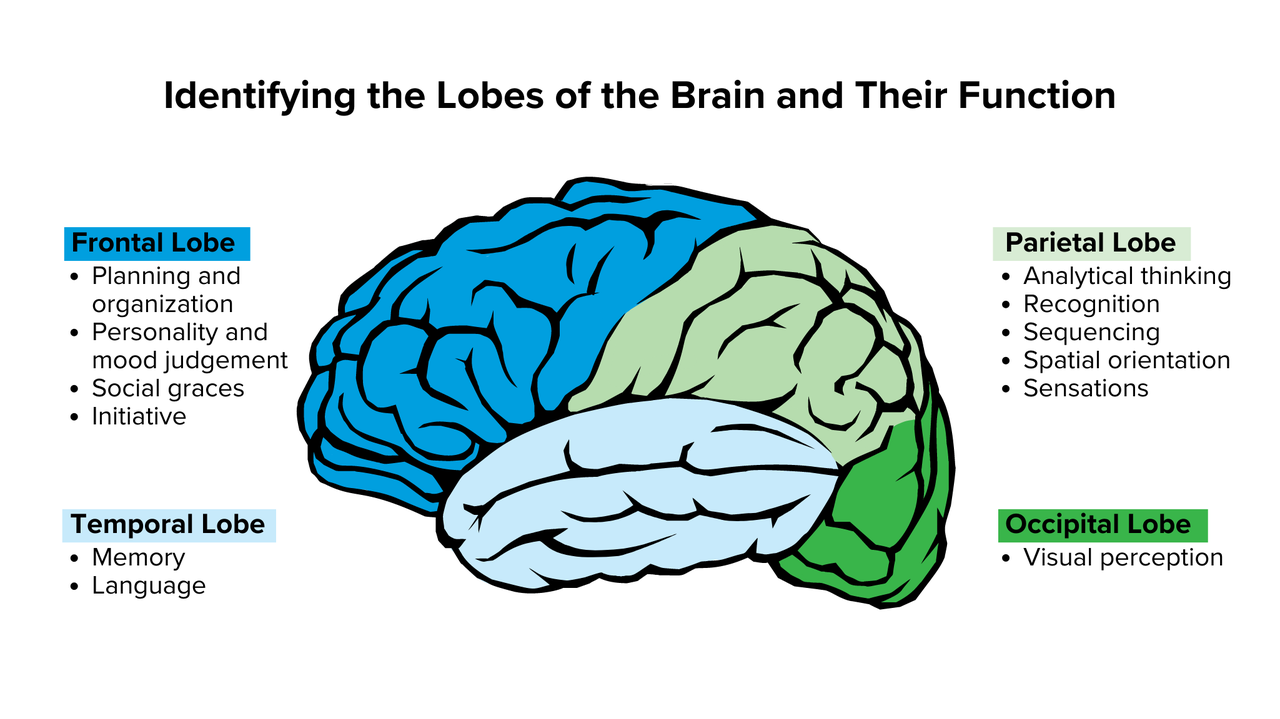
Frontotemporal lobe dementia (FTD) is an umbrella term for a spectrum of relatively uncommon disorders that primarily affect the frontal and temporal lobes of the brain.
The frontal lobes (behind the forehead) as associated with personality, behaviour, and language. The temporal lobes (on the side behind the ears) are associated with comprehension and memory. This disease is caused by the death of brain cells in the frontal and temporal lobes of the brain. Frontotemporal dementia tends to occur at a younger age and is more common when a person reaches their 60s but can occur as early as the 30s.
Signs and symptoms may vary greatly from one person to the next. There are often changes in behaviour, poor judgment, or language difficulties.
Symptoms
Behaviour changes
Speech and language problems
Movement difficulties