Talk to your doctor if you or someone close to you has symptoms of Posterior Cortical Atrophy.
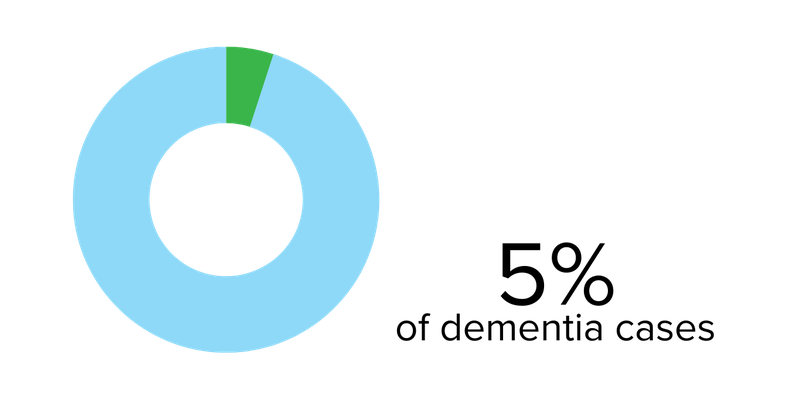
Posterior Cortical Atrophy (PCA) is a progressive and gradual degeneration of the brain’s outer layer (cortex). It happens in the back part of the brain (posterior).
The posterior cortex of the brain is responsible for processing visual information. It is unknown whether PCA is a unique disease or a possible variant of Alzheimer’s because PCA can have brain changes similar to other diseases like Lewy Body Dementia or Creutzfeld-Jackob disease. While most cases of Alzheimer’s occur in people 65 or older, the onset of PCA is often between 50 and 65.
Symptoms can vary from person to person and change as the condition progresses. In the early stages, most people do not have substantial changes regarding memory, but memory can be affected later.
Symptoms
Difficulty with visual tasks
Other symptoms